Français | Português | العربية
Page Map
Much remains unknown about the trajectory of the transmission of COVID-19 in Africa. Many fear that with its high levels of poverty, weak health systems, and crowded urban areas, the virus could be particularly devastating. Others hope that with its warmer climate, youthful population, and experience fighting infectious disease, that Africa will be able to avoid the worst of the pandemic. This analysis provides a review of relative risk factors associated with the novel coronavirus as a means of generating potential insights into the varied and at times overlapping levels of vulnerability faced by each African country.
Mapping Vulnerability by Risk Factor
Understanding the relative risks each country faces can better guide response efforts in both the introductory and subsequent stages as the pandemic evolves. Following are a series of maps graphically representing relative levels of vulnerability across the continent (scaled from 1 to 5, with 5 being greatest level of vulnerability).
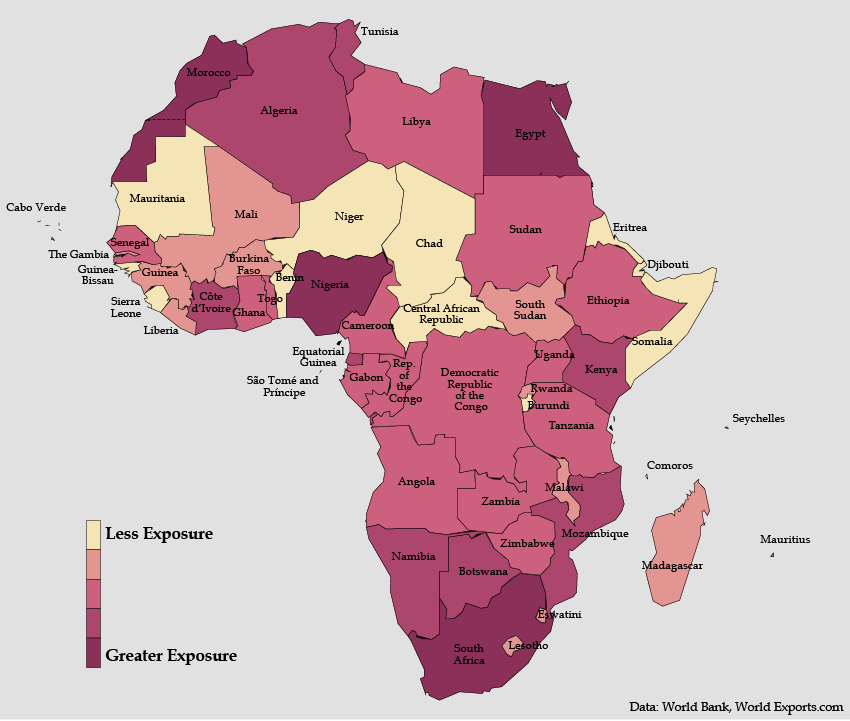
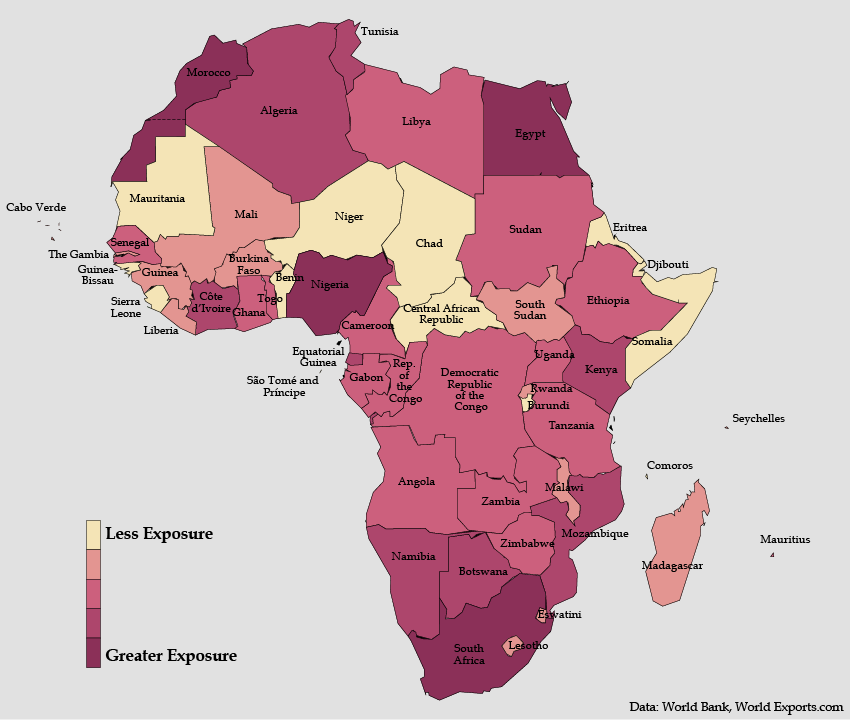
International Exposure
- As with every region of the world, the first cases of the coronavirus in Africa came from exposure to international contacts—travel, trade, tourism, or business.
- African countries with the greatest level of international contact (such as Egypt, Morocco, Nigeria, and South Africa) were among the hardest hit in the early stage of this crisis.
- While international exposure has been critical in the initial stage of the pandemic, now that the virus is on the continent, intra-continental and intra-national transmission vulnerabilities will take on increasingly greater importance.
Public Health System
- African public health systems regularly face the challenge of curbing the spread of infectious disease at the community level. The capacity of a public health system to test for COVID-19, especially in densely populated areas, is essential for identifying, isolating, and treating those infected—and thereby reducing the impact on society.
- Protecting health workers is an especially critical priority for countries with relatively weaker health systems as these skilled practitioners are integral to maintaining the capacity of these health services.
- The robustness of the public health institutions will also be vital for sharing information and best practices among public health practitioners so as to facilitate adaptation and communication with the public.
- Conversely, relatively weak public health systems are likely to face the spread of the virus without significant testing or tracking of the disease, leading to accelerated transmission and underreporting.
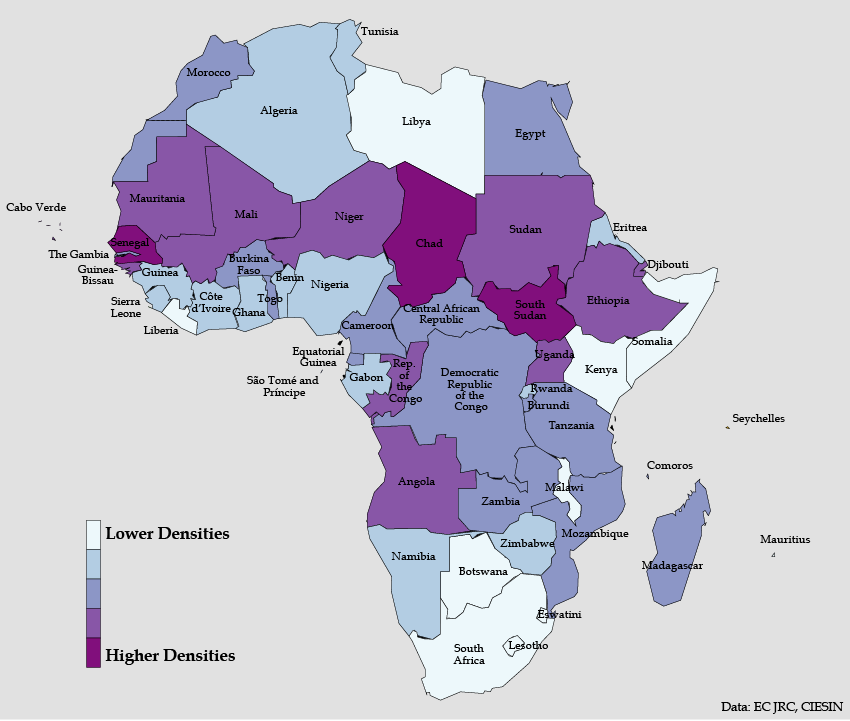
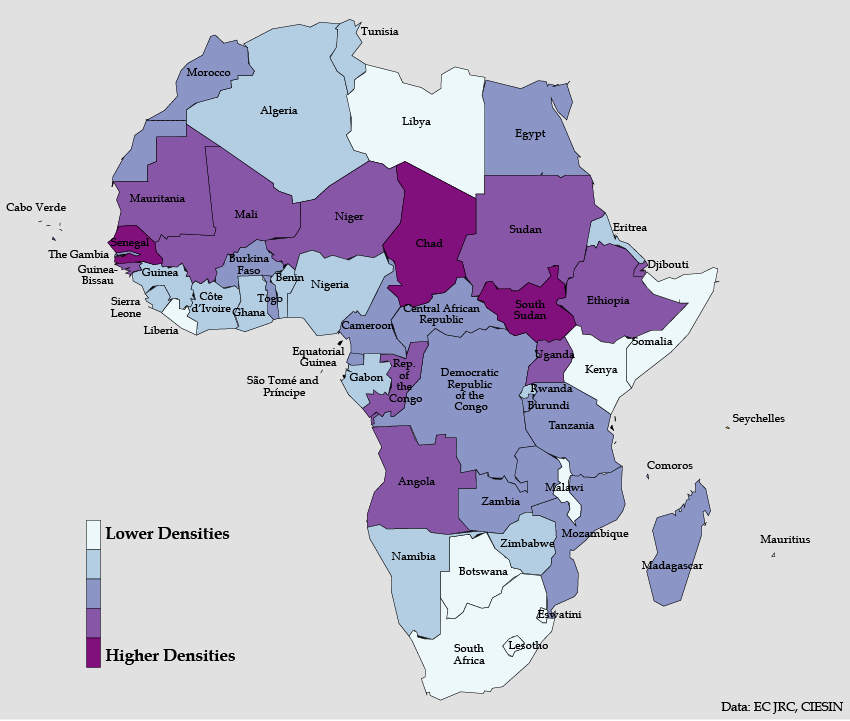
Density of Urban Areas
- Urban density measures the average number of people per kilometer living in a country’s built-up areas. It is an effective gauge of how clustered a country’s population is overall, distinct from the figure of total population.
- African urban areas are often remarkably densely populated, creating conditions where viruses can spread quickly and undetected in crowded informal settlements. Urban density is characteristic even of relatively sparsely populated countries in the Sahel, where the concentration of human settlements in capital cities creates high levels of vulnerability. A similar pattern is seen in South Sudan, where inhabited areas average 8,730 people per square kilometer.
- Urban layouts and architectures in these locations are similar to the compacted towns of Spain and Italy, where the virus has hit Europe the hardest to date.
- Built-up areas across much of Africa have higher population densities than those in Europe and the United States. Influenza transmission rates in India have been found to increase above a population density of 282 people per square kilometer. The density of many built-up areas in Africa is over five times this threshold.
Total Population in Urban Areas
- Distinct from population density of urban areas is the total number of people living in urban areas in a country. This, thus, captures all of the people at higher risk for spreading the virus, whether they inhabit less-densely populated urban sprawl or packed city centers.
- COVID-19 appears to thrive in cities where it can be transmitted quickly at close range through the movement and frequent contact between people. Countries with higher urban populations are faced with the logistical and communication challenge of informing, monitoring, and possibly isolating a larger pool of at-risk people.
- African countries with the largest urban populations all have megacities: Lagos, Cairo, Addis Ababa, Kinshasa, and Johannesburg. All of these cities, except Addis Ababa, have peak population densities greater than New York City (56,000 people per square kilometer). Cairo’s peak population density (175,000/km2) easily tops the density of Wuhan, China (106,300/km2), where the novel coronavirus originated.
- Stay-at-home orders will be particularly difficult to maintain in African cities where many residents lack adequate shelter, sanitation, and the monetary means to stock up on supplies and to stop work.
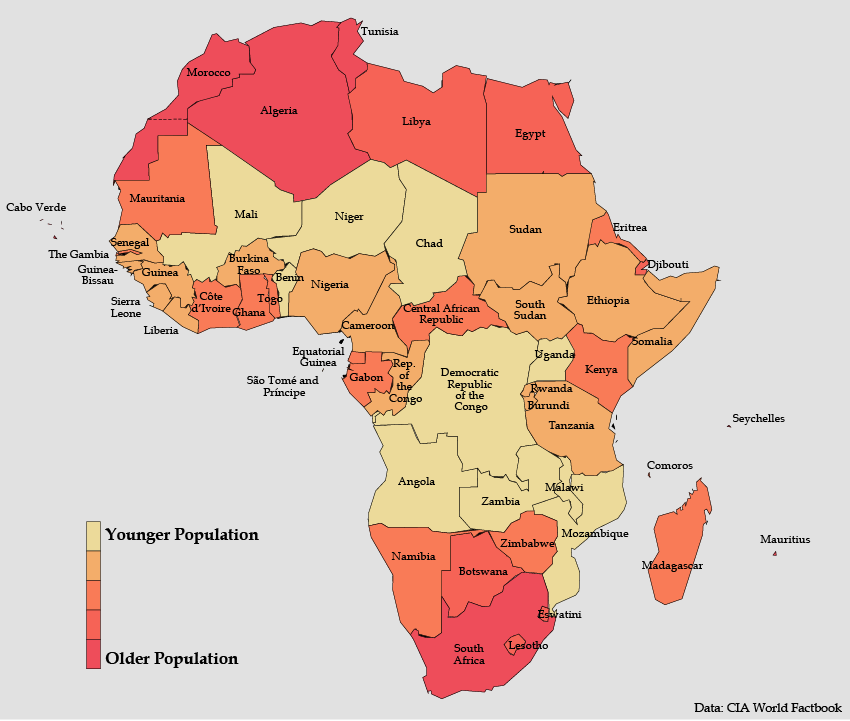
Population Age
- Approximately 80 percent of COVID-19 fatalities have been among people over the age of 60. With 70 percent of Africa’s population under the age of 30, Africa’s youth bulge may be a buffer against the most devastating human costs of the disease on the continent.
- The benefits of a more youthful population, however, will need to be balanced against other underlying health factors facing many African populations such as malaria, malnutrition, tuberculosis, and HIV/AIDS. The mortality rate per reported cases across the continent is currently 4 percent, though this varies widely by country, presumably as a result of limited testing and reporting capabilities. In South Africa, the African country with the most reported cases but also among the best capability for testing, the fatality rate is less than 1 percent.
- Many of the African countries with relatively older populations, such as the Seychelles, Cabo Verde, Mauritius, and Tunisia have lower vulnerabilities on other risk factors. This raises the prospect that fatality rates may be higher in some less vulnerable countries and underscores the importance of every country responding to its unique risk profile.
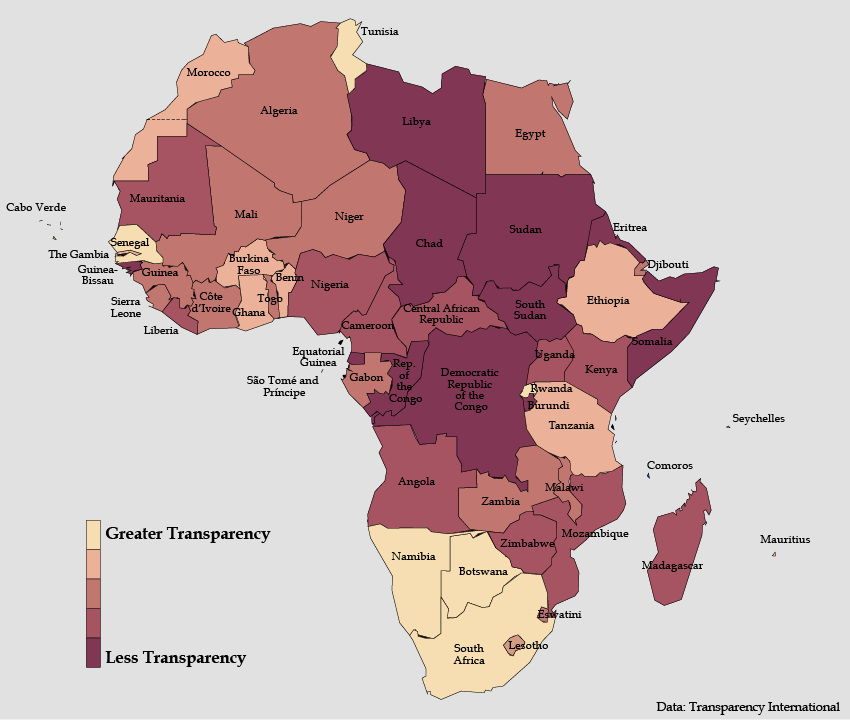
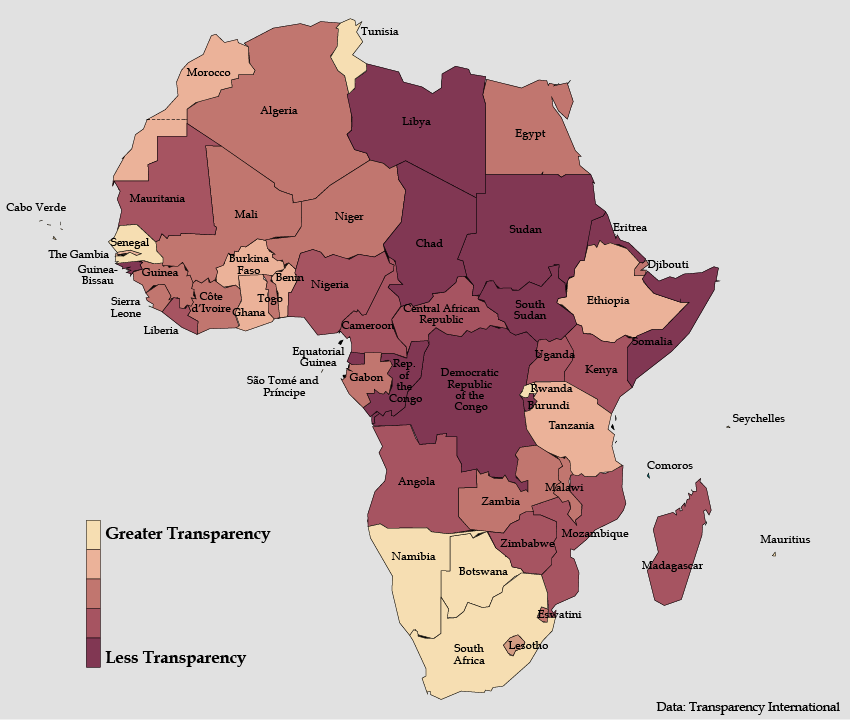
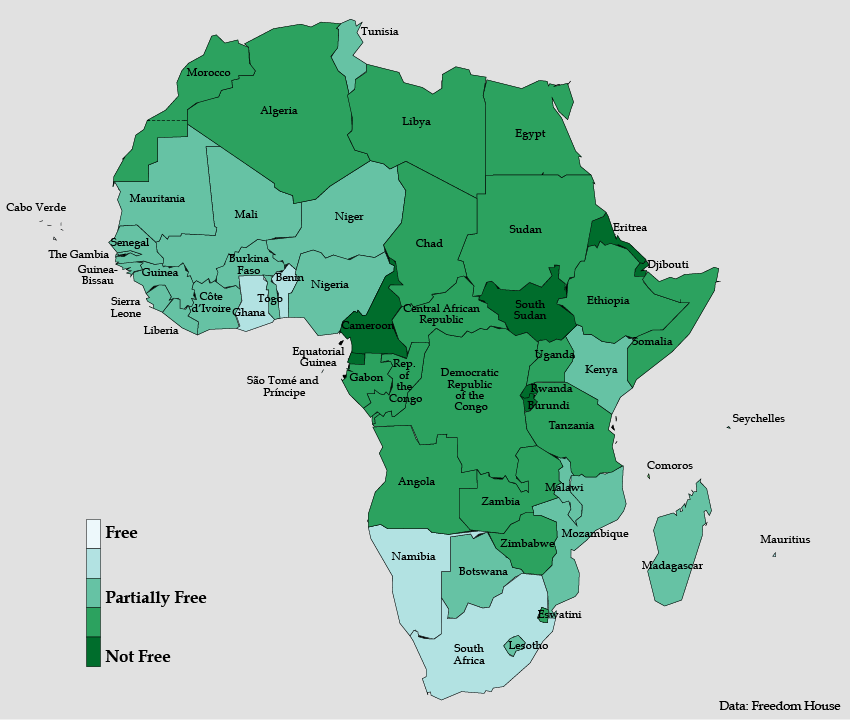
Government Transparency
- Citizen cooperation with government guidance to mitigate the effects of the pandemic is closely tied to trust in the government. A government’s reputation for transparency engenders trust and a sentiment of solidarity and reinforces a belief among citizens that restrictions are being applied fairly.
- If the public or international bodies do not trust the data on transmission rates, then they are less likely to cooperate, contributing to alternate narratives of the severity of the disease.
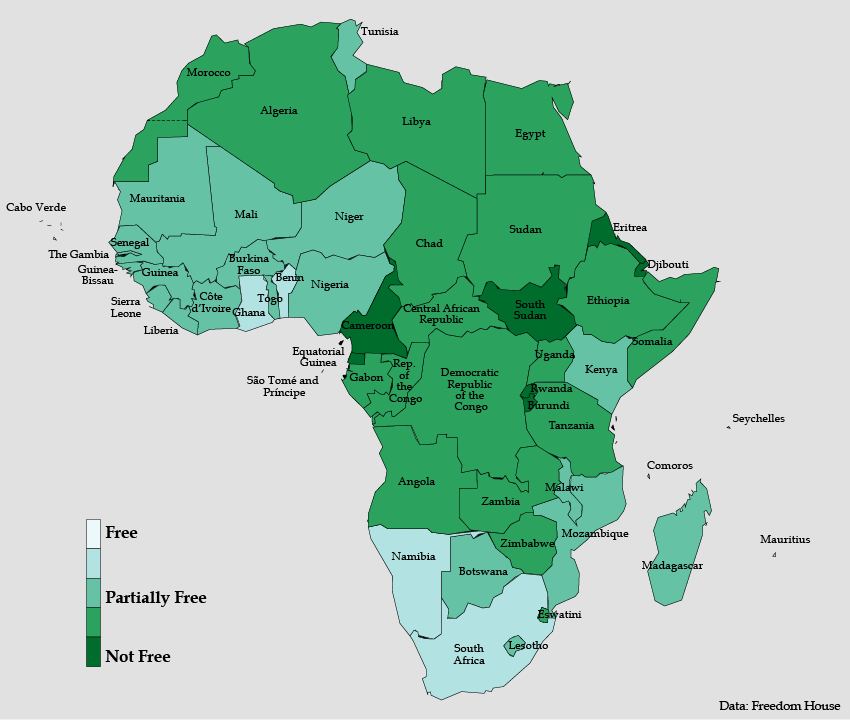
Press Freedom
- A free press serves as an unparalleled early warning system for a society in times of emergency, sharpening focus on the severity of a problem and prompting an urgent government response.
- Independent media play an indispensable role in informing the public and validating government pronouncements, especially in times of crisis.
- Media also help hold governments accountable for transparent reporting of key data about a crisis and forcing the government narrative to mirror reality.
- Government arrests of journalists under the pretext of emergency powers is self-defeating because it undermines the credibility of the government.
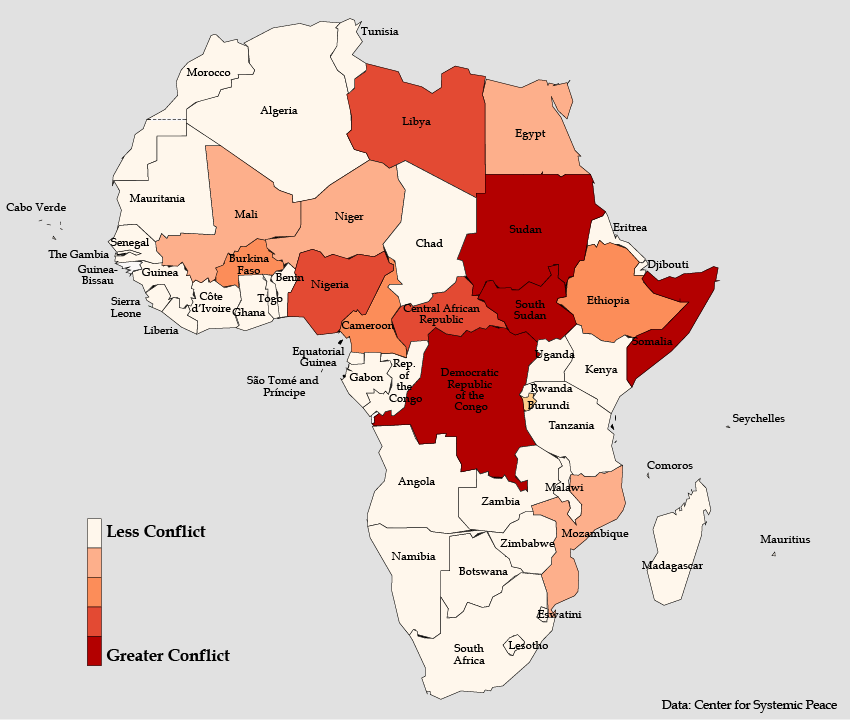
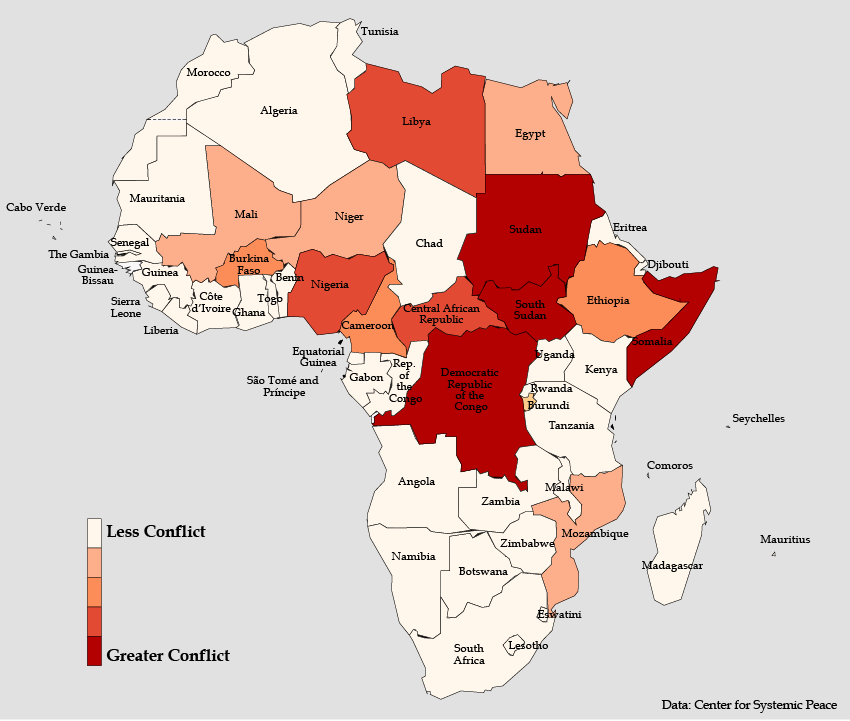
Conflict Magnitude
- Armed conflict disrupts public health systems in affected areas and limits access to basic goods like food, water, and medical supplies.
- The degree of intensity and geographic spread of conflict shapes the level of disruption caused for a society.
- Conflict-affected populations are also often starting from higher levels of vulnerability with fewer resource buffers than other populations, making the impact of exposure to an infectious disease all the more severe.
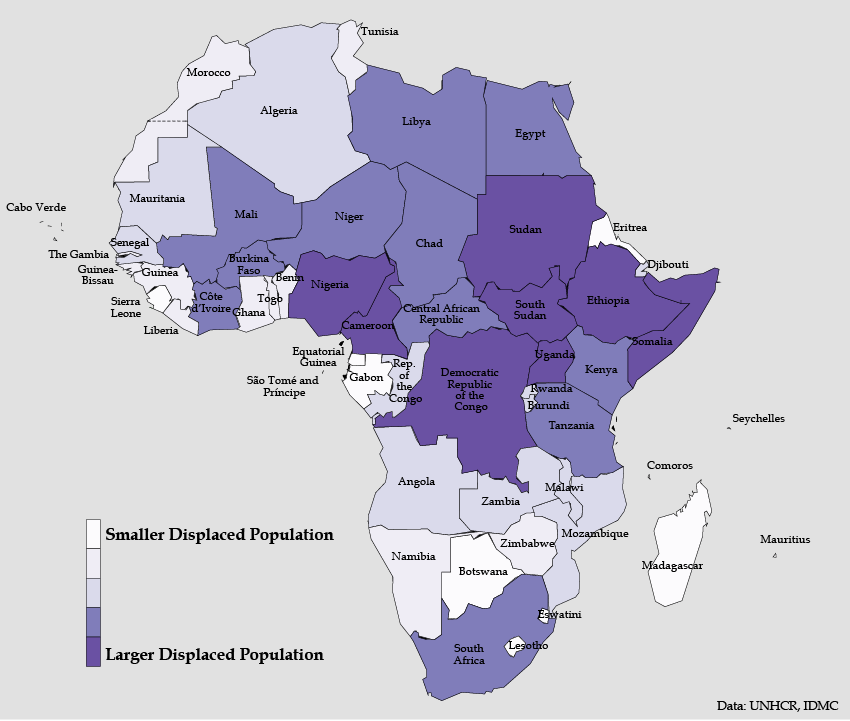
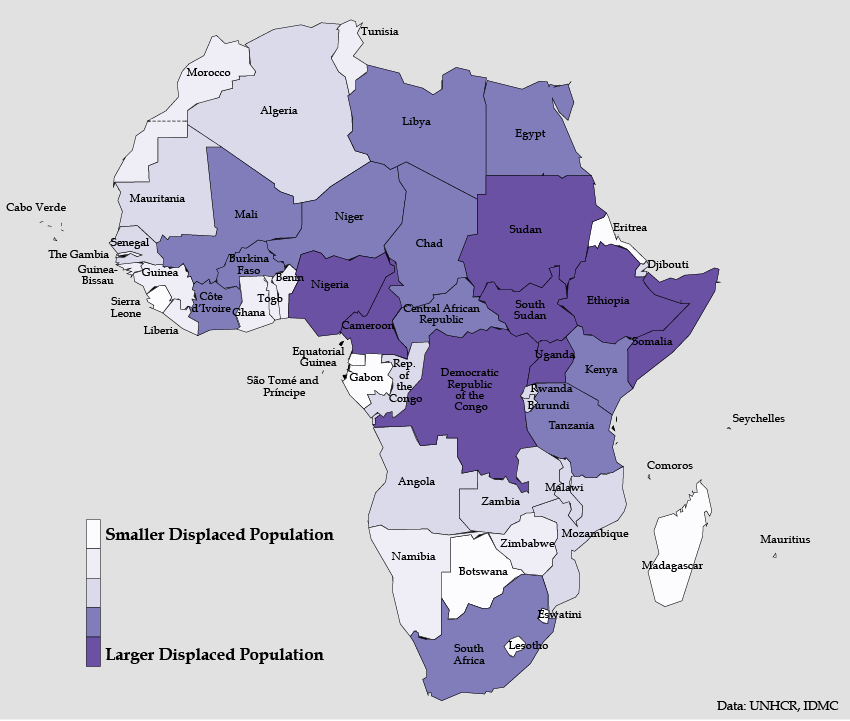
Displaced Populations
- Refugees and internally displaced populations may be congregated in large camps with inadequate access to water, soap, or sanitation. Health services are often overstretched and inaccessible.
- The close quarters typical of such settlements greatly facilitates the spread of any infection once it is introduced.
- Eighty-five percent of Africa’s 25 million forcibly displaced persons are concentrated in 8 countries: the Democratic Republic of the Congo (DRC), South Sudan, Somalia, Ethiopia, Sudan, Nigeria, the Central African Republic (CAR), and Cameroon.
Composite Chart of Risk Factors
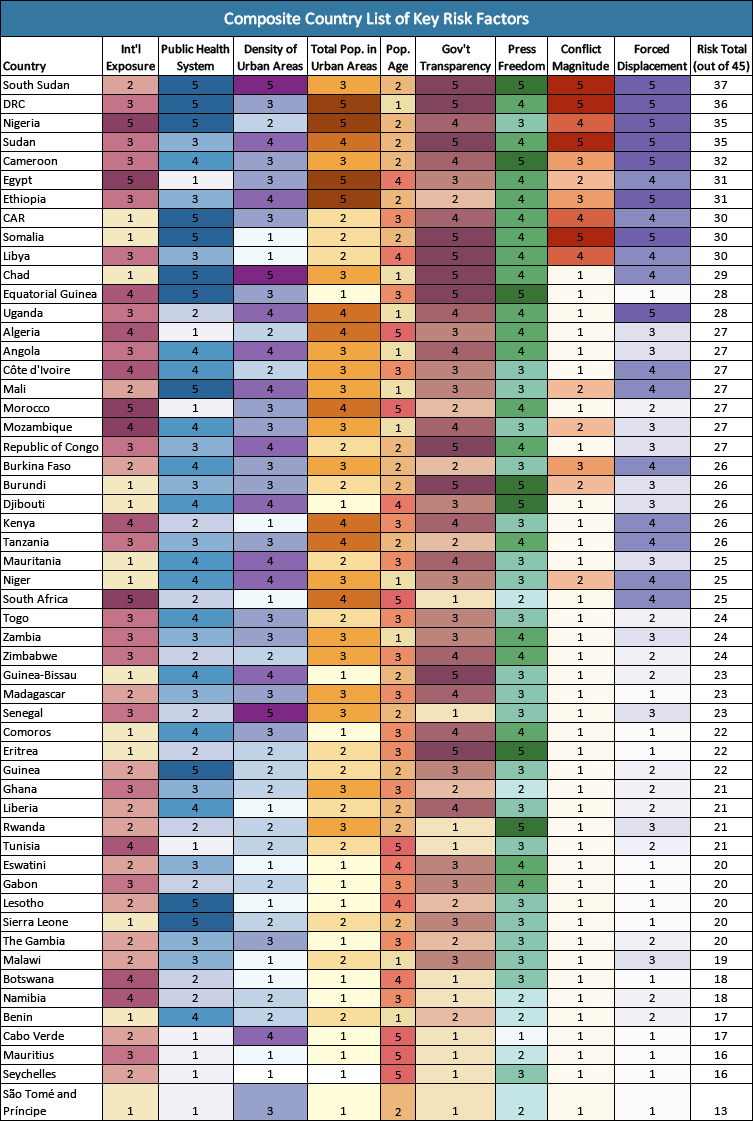
Note: Countries are categorized by relative risk for each factor on a 1 to 5 scale, with 1 representing less risk and 5 most risk.
Examining the compiled list of nine risk factors considered reveals that a handful of countries—South Sudan, the DRC, Sudan, and Nigeria—are at or near the highest category of risk for nearly all of the risk factors. This multilayered risk portfolio underscores the vulnerability these countries face and the importance of trying to identify and limit the spread of the virus at the early stages before it becomes entrenched in the high density urban or displaced person areas.
Notably, with the exception of Nigeria, these countries are not among those with the highest levels of international exposure, providing them a brief window to ramp up containment measures. Key to these efforts will be enhanced and transparent public communications regarding COVID-19, public health guidance, and candid information about what the government is doing and what individuals should do if they exhibit symptoms. For some of these countries, given their constricted space for sharing information, this will require significantly improved levels of transparency and space for independent media.
Another tranche of countries—Cameroon, Ethiopia, Chad, Somalia, Uganda, Egypt, and CAR—are just below the highest composite risk category. These countries also exhibit multiple layers of vulnerability across the nine risk factors considered and would need to focus on mitigating their areas of risk, to the extent possible, while drawing on their relative strengths. Again, with the exception of Egypt, none of these are in the first order of African countries facing the highest levels of reported cases in the first stage of transmission from international exposure.
Fortunately, there are a number of countries in the bottom third of the chart that have relatively fewer high-risk vulnerabilities and a number of positive factors in their favor. Many benefit from having less dense and smaller urban populations. These countries will certainly need to remain vigilant, as the impacts in China, Europe, and the United States have shown. However, this cohort of African countries is starting from a stronger position than others, and with early identification and isolation of cases, may be better able to minimize the worst effects of this pandemic.
Risk Factors Linked to Initial Stage of Reported Cases
While each risk factor is relevant depending on the context, the pattern of reported cases for the onset of COVID-19 in Africa is highly correlated with just a few: international exposure, size of urban population, and strength of health sector. The latter, importantly, reflects the capacity to conduct timely testing. This underscores the pertinent reality in Africa (and elsewhere) that reported cases only reflect that part of the problem that is visible. In fact, cases of the coronavirus may be widespread elsewhere, though they are not identified and reported.
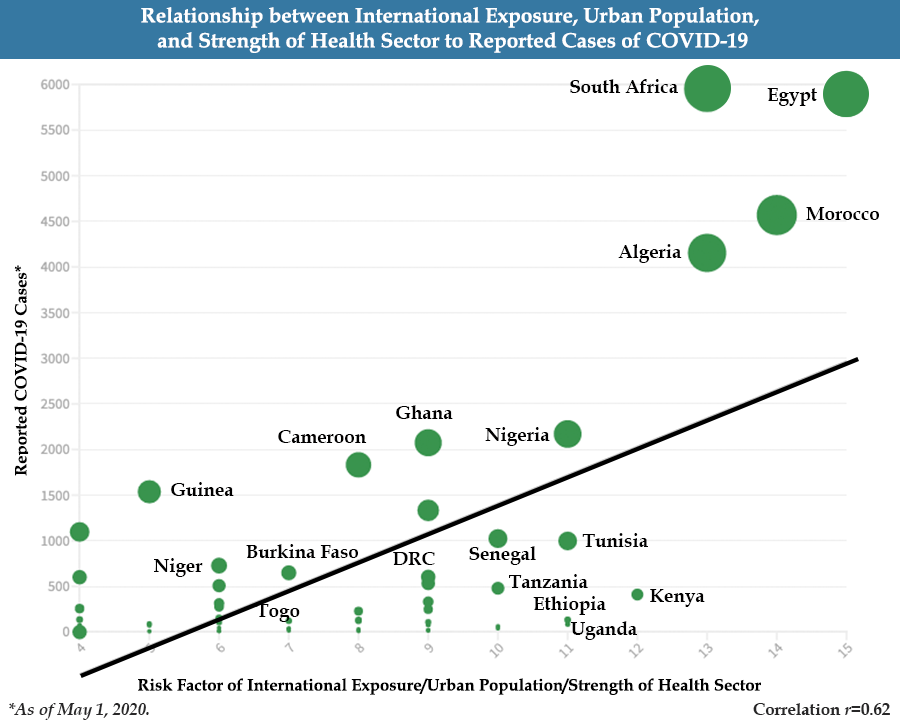
The strong correlation shows the influence of international exposure on generating initial cases. This is why Egypt, South Africa, Morocco, and Nigeria saw some of the first episodes of the virus. Their large urban populations and relative ability to test and report cases, subsequently, led to the sharp growth in cases seen in these countries. Notably, Kenya, Nigeria, Ethiopia, Uganda, Tanzania, and Zimbabwe are countries that exhibit relatively high risk factor scores for rapid increases in initial transmission as well, though they have not seen the high levels of reported cases. (See table below of countries with highest risk on the international exposure, strong public health systems, and total urban population factors). This may reflect relatively effective efforts to contain the spread of the virus—or lagged reporting of cases. Accordingly, these countries will be important to watch.
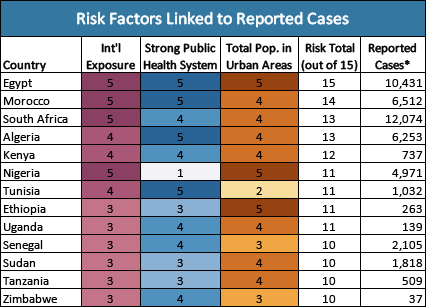
*As of April 1, 2020.
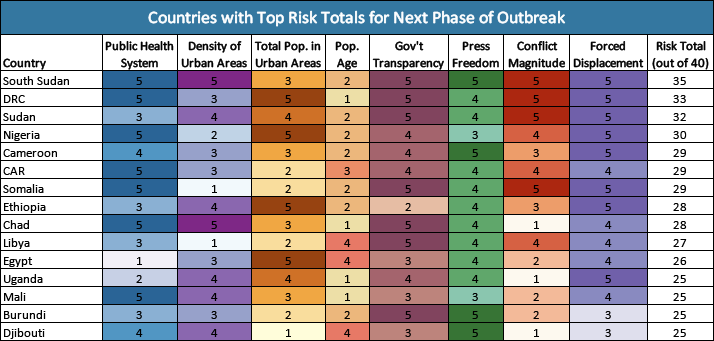
Assessment of Risk Factors for Next Phase
While international exposure, size of urban population, and capacity for testing may drive the reported number of cases initially, subsequent stages are likely to also exploit other vulnerabilities such as weak health systems, densities of urban populations, conflict, size of displaced populations, trust in government, and openness of communications channels.
Moving forward, therefore, it will be important to keep an eye on countries with high composite vulnerabilities and not just those with relatively higher numbers of reported cases currently. In considering this composite calculation, countries such as South Sudan, DRC, Sudan, Cameroon, CAR, Somalia, and Chad appear to be particularly vulnerable to impacts from COVID-19 as it moves into these populations. Likewise, despite not having the continent’s largest total urban populations, countries in the Sahel and Great Lakes regions appear to be at high risk for severe outbreaks. Attention in these countries, however, would need to be relatively more focused on densely populated cities and towns, supporting public health institutions, and strengthening the transparency of public information sharing. Again, however, each country faces a unique mix of vulnerabilities that will require a customized response.
Additional Resources
- Shannon Smith, “Managing Health and Economic Priorities as the COVID-19 Pandemic Spreads through Africa,” Spotlight, Africa Center for Strategic Studies, March 30, 2020.
- Africa Center for Strategic Studies, “Five Myths about Coronavirus in Africa,” Spotlight, March 27, 2020.
- Wendy Williams, “COVID-19 and Africa’s Displacement Crisis,” Spotlight, Africa Center for Strategic Studies, March 25, 2020.
- Africa Center for Strategic Studies, “Coronavirus Spreads through Africa,” Infographic, March 19, 2020 (updated daily).
- Shannon Smith, “What the Coronavirus Means for Africa,” Spotlight, Africa Center for Strategic Studies, February 4, 2020.
- Johns Hopkins University Center for Systems Science and Engineering COVID-19 Global Cases
- World Health Organization Coronavirus Information
- Africa Centres for Disease Control and Prevention
More on: COVID-19 Health & Security


 ⇓
⇓

 ⇓
⇓ ⇓
⇓